What Is TMS Treatment for Depression?
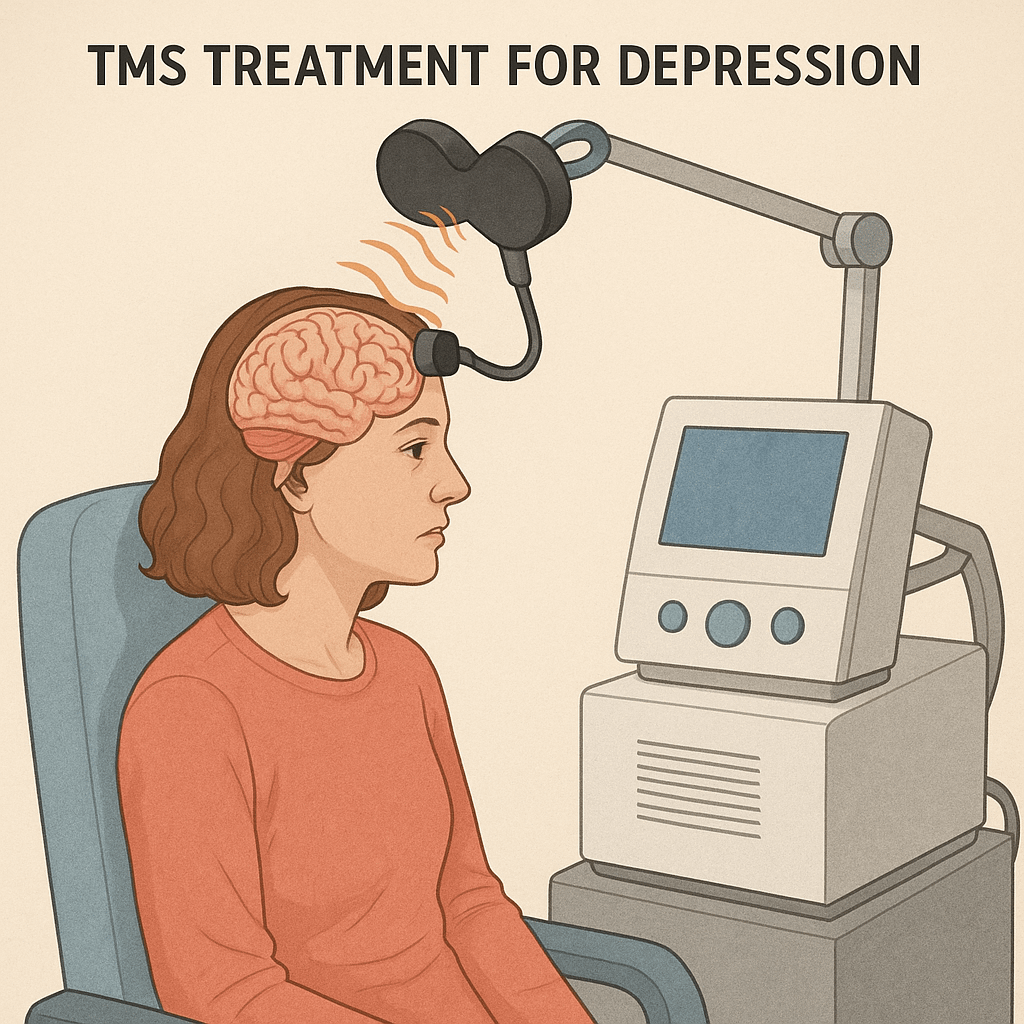
TMS treatment for depression, also known as Transcranial Magnetic Stimulation, is a groundbreaking, non-invasive therapy designed to treat individuals suffering from major depressive disorder. It works by sending magnetic pulses through the scalp to stimulate specific areas of the brain involved in mood regulation.
Unlike traditional antidepressants or electroconvulsive therapy (ECT), TMS doesn’t require surgery, anesthesia, or systemic drugs. The U.S. Food and Drug Administration (FDA) approved TMS in 2008 for patients with treatment-resistant depression. Today, it’s a popular option for people who’ve tried everything else without success.
How TMS Treatment for Depression Works
The human brain relies on electrical impulses to function. In people with depression, certain regions, especially the prefrontal cortex, often show reduced activity. TMS targets these areas directly using magnetic fields, increasing neural activity and helping restore emotional balance.
A typical TMS session involves:
- A magnetic coil placed gently on your head
- Repetitive pulses are delivered for 20–40 minutes
- A full course spanning 4–6 weeks, with five sessions per week
There’s no pain involved, though some patients report a tapping sensation or mild scalp discomfort.
Why TMS Treatment for Depression is a Game-Changer
Many people turn to TMS after trying multiple medications that either didn’t work or caused too many side effects. Here’s why TMS stands out:
- Drug-Free: No chemicals altering your entire system
- Minimal Side Effects: No weight gain, nausea, or sexual dysfunction
- High Success Rate: Over 50% of treatment-resistant patients see significant improvement
- Long-Term Results: Benefits can last months or even years with occasional maintenance sessions
For many, it’s the first time they’ve experienced life without the heavy fog of depression.
Who Should Consider TMS Treatment for Depression?
Not everyone is eligible for TMS, but many are. Ideal candidates include:
- Adults diagnosed with Major Depressive Disorder (MDD)
- Individuals who haven’t responded to at least one antidepressant
- People who experience side effects from medications
- Patients who are not at risk of seizures and don’t have metal implants in the head
Before starting, you’ll go through a thorough evaluation with a psychiatrist to determine if TMS is right for you.
What to Expect During TMS Treatment for Depression
TMS therapy is an outpatient procedure, and you don’t need to change your daily routine. Here’s a quick look at what happens:
- Consultation and Mapping: A specialist maps your brain to identify the stimulation target.
- Daily Sessions: You’ll visit the clinic five times a week.
- Comfortable Experience: Sit in a recliner, wear the coil, and relax.
- Short Recovery: You can return to work, drive, or run errands immediately after.
Most patients begin to notice improvement after 2–3 weeks.
Side Effects and Safety Profile
TMS treatment for depression is considered extremely safe. Common side effects are mild and usually go away on their own:
- Headaches (in the first few sessions)
- Scalp sensitivity
- Lightheadedness
- Jaw or facial twitching during pulses
Serious complications, such as seizures, are infrequent, occurring in less than 0.1% of cases. Clinics follow strict safety guidelines, making the treatment highly controlled and predictable.
Success Stories: TMS Treatment for Depression in Real Life
Many patients describe TMS as life-changing. Real people have gone from feeling stuck and hopeless to regaining joy, motivation, and social connection. Clinical trials show:
- 60% of patients report a significant decrease in symptoms
- 30–40% reach complete remission
- Improvements often persist for up to a year or longer
Stories like “I finally felt like myself again” or “TMS gave me my life back” are common in review boards and clinic testimonials.
How TMS Compares to Other Treatments
| Treatment | Invasiveness | Side Effects | Success Rate | Recovery Time |
| Antidepressants | None | Systemic, ongoing | 40–60% | Immediate |
| Talk Therapy | None | Emotional fatigue | Variable | Immediate |
| ECT | Invasive | Memory loss, sedation | 70–80% | Requires recovery |
| TMS Therapy | Non-invasive | Mild, short-term | 50–60% | None |
TMS fills a critical gap—high efficacy with fewer downsides.
Cost of TMS Treatment for Depression
The cost can vary based on location and provider, but a typical full course ranges between $6,000 and $12,000.
Most insurance providers cover TMS if you meet the criteria:
- Treatment-resistant depression diagnosis
- Failed 1–4 antidepressant trials
- Documentation from your psychiatrist
Major insurers, including Aetna, Blue Cross Blue Shield, Medicare, and UnitedHealthcare, offer partial or full reimbursement.
TMS in Teens and Seniors
TMS is currently FDA-approved for adults 18 years of age and older. However, researchers are actively studying its use in adolescents and older adults:
- Teens: Early trials suggest it’s safe and potentially effective for treatment-resistant depression.
- Seniors: Especially beneficial due to the avoidance of drug interactions and cognitive side effects.
Clinical trials are underway to expand official guidelines and offer this therapy across all age groups.
The Science Behind the Therapy
TMS works because of neuroplasticity, the brain’s ability to adapt and change. By stimulating areas involved in mood and behavior, it encourages healthier neural patterns.
Research shows TMS increases blood flow and boosts the release of dopamine and serotonin, neurochemicals often lacking in people with depression.
It’s like rebooting your brain without needing to rewire it from scratch.
Common Myths and Facts About TMS
| Myth | Fact |
| TMS is the same as electroshock therapy | TMS is magnetic, not electrical, and is pain-free |
| It alters your personality | TMS restores brain function—it doesn’t change who you are |
| It’s only for severe cases | It’s ideal for moderate to severe depression |
| You’ll need it forever | Many patients experience long-term relief |
The Future of TMS Treatment for Depression
TMS technology is evolving fast. Future innovations include:
- AI-assisted targeting: More precise brain maps
- Wearable home-use devices: In early development
- Deeper brain stimulation: Using newer coil designs
- Personalized protocols: Tailored to your brain’s unique patterns
Soon, TMS may be part of early-stage treatment plans instead of a last resort.
Frequently Asked Questions
1. How soon will I feel results?
Some patients experience improvement within 2 weeks, but the full benefits typically appear after 4–6 weeks.
2. Is TMS therapy painful?
No, but you may feel a tapping sensation. It’s generally well-tolerated.
3. Can I stop taking medication during TMS?
Possibly—but only under medical supervision.
4. Will I need booster sessions?
Some people benefit from follow-up sessions every few months.
5. Does TMS work for anxiety?
It’s not FDA-approved for anxiety alone, but many patients report decreased anxiety symptoms.
6. How long do the results last?
Many patients enjoy lasting relief for 6 months to 1 year, or more, with maintenance.
Conclusion: Is TMS the Right Step Forward?
TMS treatment for depression represents one of the most promising, least invasive, and most effective tools we have today. For individuals who’ve hit a wall with traditional methods, it offers real hope, without relying on lifelong medication or drastic procedures.
If you or someone you love is struggling with depression, now might be the time to explore TMS therapy with a trusted mental health provider.
